Radiculopathy Symptoms & Treatment Options
What is Radiculopathy ?
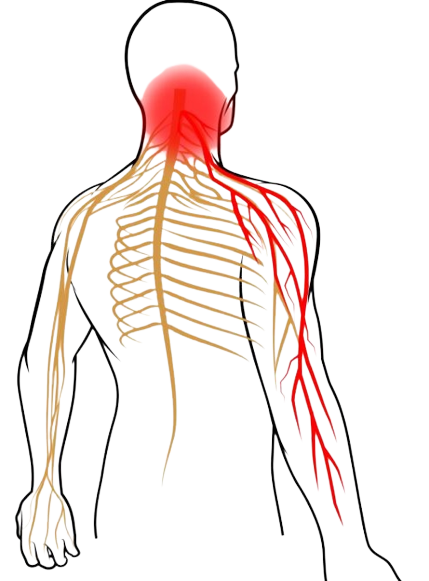
The spine is made up of many bones called vertebrae. In addition, the spinal cord runs through a canal in the center of these bones. From this cord, nerve roots split and travel between the spinal bones and various parts of the body. When these nerves become damaged or pinched, the resulting condition is called radiculopathy (also known as a pinched nerve).
This condition can have different names based on where it occurs in the spine, such as:
Lumbar Radiculopathy: Occurs in the lower back and often involves spine nerves that travel into the sciatic nerve (See sciatica). This is the most common form of the condition.
Cervical Radiculopathy: This happens when a nerve root in the neck becomes compressed. Symptoms usually occur in the arms and hands, as these are the areas affected by this portion of the spinal cord.
Thoracic Radiculopathy: Caused by a compressed nerve root in the upper back. Patients often feel numbness and pain that wraps around to the front of the body. This is the least common location for pinched nerves.
Causes & Risk Factors
Radiculopathy normally occurs when there are changes in the tissues surrounding the nerve roots. These tissues include tendons, intervertebral discs, and spinal vertebrae. When these tissues change in size or shift in position, the space where the nerve roots travel inside the spine narrows. These openings are called foramina. When the foramina narrow, it causes foraminal stenosis, which is very similar to spinal stenosis. In most cases, gradual degeneration of the spine causes foraminal stenosis as we age. That being said, spinal injury can also cause foraminal stenosis.
Herniated Discs
Herniated or bulging discs are the most common cause of Radiculopathy. Spinal discs act as cushions between the vertebrae, but on occasion they may slip out of place or become damaged. This can put pressure on nerves and can affect areas in the lower back as well as the neck.
Bone Spurs
Bone spurs are areas of extra bone growth and this can lead to the narrowing of spinal passageways. This can also cause radiculopathy. Bone spurs form in the spine due to inflammation from trauma, osteoarthritis, or other degenerative conditions.
Other Causes
Thickening of the spinal ligaments can narrow spinal passageways and lead to nerve compression. Though not as common, spinal infections and various cancerous or noncancerous growths in the spine and its joints can press against nerve roots like a synovial cyst. Radiculopathy can also occur in patients who have a family history or genetic predisposition to the condition. Lastly, repetitive improper movements can contribute to the formation of pinched nerves. Such movements occur in those who participate in high-impact sports, heavy lifting, or manual labor or in patients with unstable segments of the spine.
Diagnosis
More often than not, the patient will need to give their physician a brief medical history. This should give the doctor enough clues to know where to start. After the medical history has been taken, it is usually followed up with physical tests. Physical examinations and tests are used to check the patient’s muscle reflexes and strength. Any pain experienced during a given movement will provide the doctor with clues about the location of the affected nerve root. In some cases, it may be necessary to use imaging tests, such as a CT scan or an MRI. These tests are used to better visualize the structures within the problem areas. In specific occasions, a nerve conduction study or an electromyography (EMG) can help determine whether the problem is muscular or neurological.
Complications of Surgery
With spine surgery, sometimes nerves can be expose to significant traction or retraction in order to gain access to spaces and achieve surgical goals. In rare instances patients suffer from radiculopathy as a consequence of surgery or when implants migrate into nerve spaces.
Recovery
After surgery, the patient will normally stay in the hospital for 1-2 days. This varies, however, based on the type of surgery and condition you have. Due to the minimally invasive nature of the procedures, scarring is often minimal. Less pain is also felt during recovery as the muscles are moved instead of cut. NSAIDs are recommended for those who still feel pain after treatment. Most patients find that they can eat and walk on the first day after surgery. Solid foods may be difficult to swallow for a few weeks if the neck was the affected area. Hoarseness is also common.
Management of patients with Radiculopathy
Normally, more conservative treatments are recommended first, such as muscle relaxants, physical therapy, steroid injections, and weight loss regimens. If these options have not given the patient sufficient relief, then surgery may be the next best alternative. That being said, some situations may restrict an individual from receiving surgical care. Patients with spinal infections, serious vertebral instability, or other serious medical conditions are a few possible examples. Working with a qualified physician to examine your condition is the only way to know if surgery is right for you. To learn more, contact us to schedule appointment with our spine specialist today!
General Radiculopathy symptoms
- Neck or Low back pain with limb radiating symptoms.
- Nerve dysfunction with extreme pain
- Lack of strength.
- Numbness, Tingling
- Inability to feel hot or cold temperature in the affected nerve area
- Inability to move without pain.
- Weakness and inability to grasp ( cervical) and Walk ( lumbar).
- Lack of rest.
- Twitching of muscles and atrophy or loss of muscle mass
More about Dr. Matin
Radiculopathy Symptoms & Treatment Options
Radiculopathy pain can be treated by Dr. Martin, give us a call to schedule an appointment.
We will provide different options of treatment.
Laminectomy
The laminae are thin bones that encase the spinal cord and nearby nerves. Sometimes, this passageway narrows as we age, resulting in pinched nerves. Laminectomy is the removal of portions of these bones allowing for more space and less pain.
Microdiscectomy
Sometimes, disc herniation can cause pressure on adjacent nerves, leading to pain or other distressing symptoms. An Microdiscectomy is a minimally invasive procedure that removes a portion of the affected disc to relieve pain
Foraminotomy
The foramina are canals that reside in-between each vertebra of the spine. A number of conditions can cause these passageways to narrow, causing nerve pain, compression, or incapacitation. A Foraminotomy ( opening of the Foramen) creates space, removes nerve pressure to treat these symptoms
Anterior Cervical Discectomy & Fusion
(ACDF) is a minimally invasive procedure that treats damaged cervical discs. Using small, specialized instruments, a surgeon will remove a portion or the entirety of the damaged disc. Bone spurs and foraminal narrowing can also be treated during this procedure.